
Sleep Apnea
“Sleep apnea is a traumatic brain injury.”
Intermittent pauses in breathing during sleep characterize sleep apnea. The breathing lapses can fragment sleep and reduce oxygen supply, leading to sleep and brain health consequences. Sleep apnea affects children and adults, men and women.
What we offer at Sleep and Brain
At Sleep and Brain, we conduct a detailed clinical history to detect the subtle symptoms of sleep-disordered breathing. We prudently search for clues during your sleep and wake period, as exampled below:
Sleep
Snoring
Bruxism
Sweating
Cold hands and feet
Drooling
Clenching
Dry Mouth
Nocturia
Wake
Sleepiness
Fatigue
Impotence
Anxiety
Depression
Irritability
Forgetful
Inattention
When you think of the term sleep apnea, you are likely considering obstructive sleep apnea. However, there are other types of sleep-disordered breathing. We discern the various types of sleep-disordered breathing, such as:
Snoring
Respiratory noise typically occurring during inspiration
Obstructive sleep apnea
Intermittent lapses in breathing due to a physical obstruction
Central sleep apnea
Intermittent lapses in breathing due to faulty brain signals in the absence of a physical obstruction
Hypoventilation syndrome
Insufficient sleep-related ventilation with high carbon dioxide levels
Hypoxemia syndrome
Low sleep-related oxygen saturations
Following a thorough history, we conduct a specialized physical examination, as exampled below, to help determine the etiology of your sleep-disordered breathing:
Obstructive sleep apnea
Facial dimensions
Dental occlusion
Tongue endurance and strength
Nasal resistance
Central sleep apnea
Peripheral edema
Shortness of breath
Hypoventilation syndrome
Obesity
Muscular weakness
We give additional considerations to medical conditions that may increase the risk for sleep-related breathing disorders. Hormone conditions like hypothyroidism (low thyroid hormone) and acromegaly (high growth hormone) may increase OSA risk by causing airway tissue swelling and obesity. Stroke and brain tumors and infections can damage the brain stem and cause central sleep apnea. Heart failure can cause a special type of central sleep apnea called Cheyne-Stokes respiration. Obesity and opioids can reduce ventilation. Consequently, we may recommend laboratory tests, imaging, and echocardiograms.
Sleep and Brain aims to identify a disease process, establish a differential diagnosis, determine an etiology, and render treatment options to ensure optimal health. We gather as much information as possible through a comprehensive exam, data collection, and photography.
Radiographic imaging using Cone Beam CT offers insight into causes and treatment solutions by visualizing anatomy. CBCT provides detailed images of the jaw, teeth, upper airway, nasal cavity, and sinuses. The best clinical outcomes occur when we can see what is happening.
The Sleep and Brain Cone Beam CT case images below illustrate an unmatched diagnostic precision and clinical expertise.

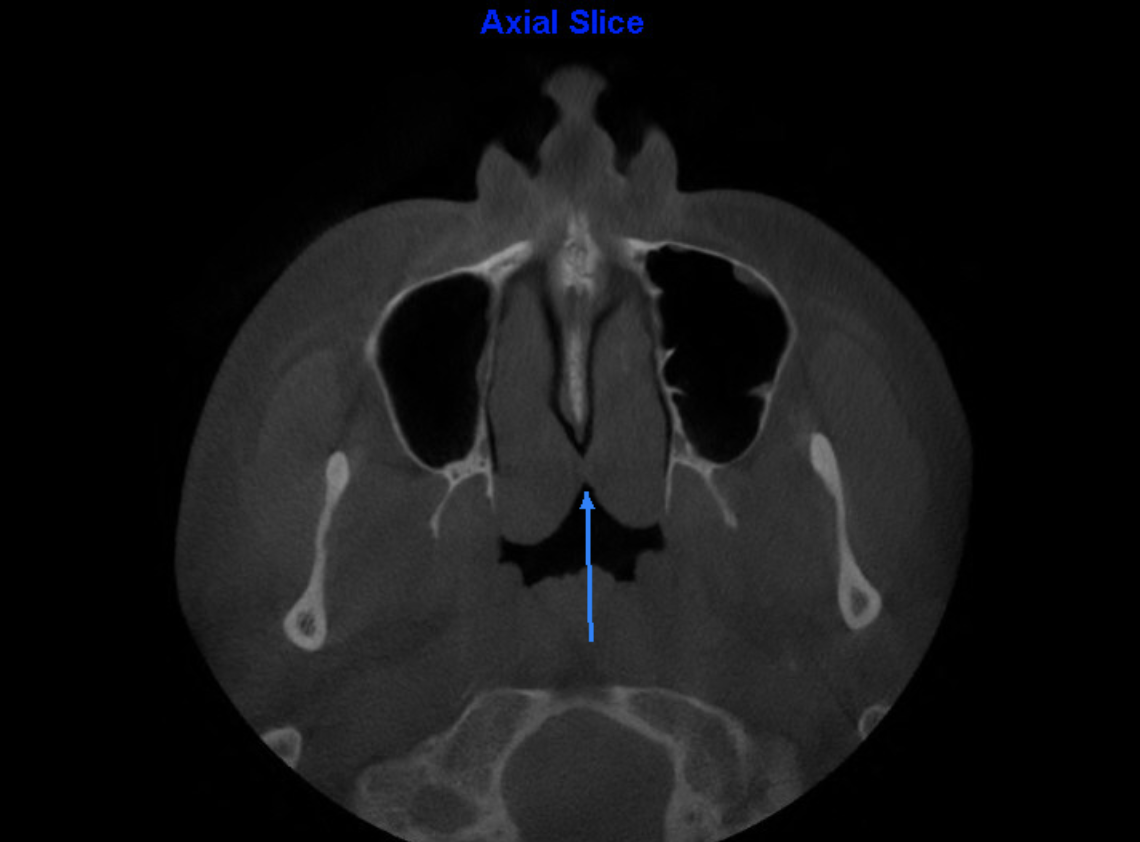
Enlarged Inferior Turbinates Touching and Obstructing the Posterior Nasal Passage

Severely Deviated Septum

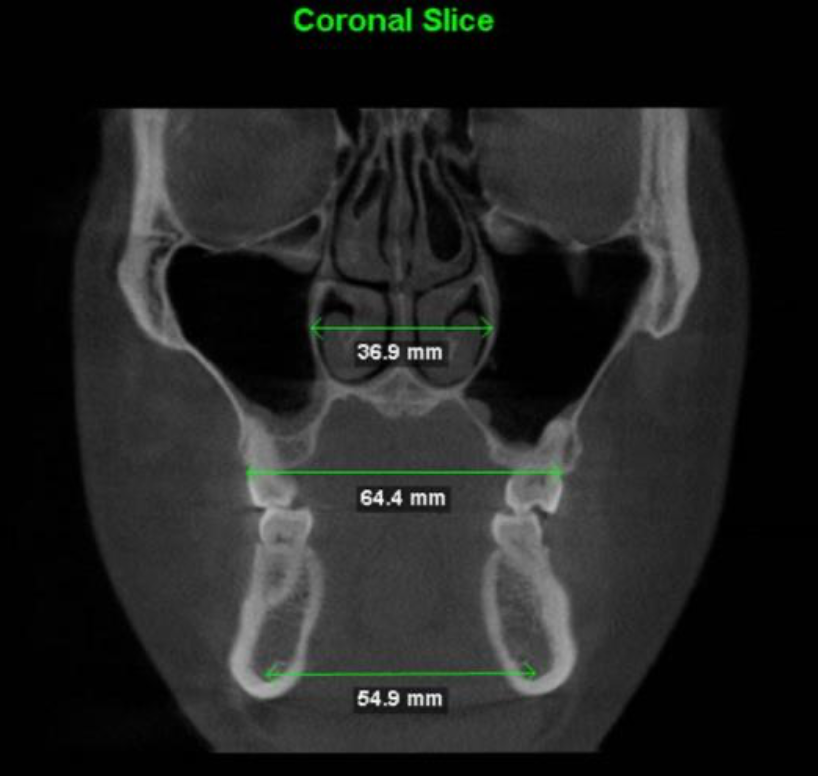
Concha Bullosa: Air Filled Medial Turbinate Causing Nasal Obstruction
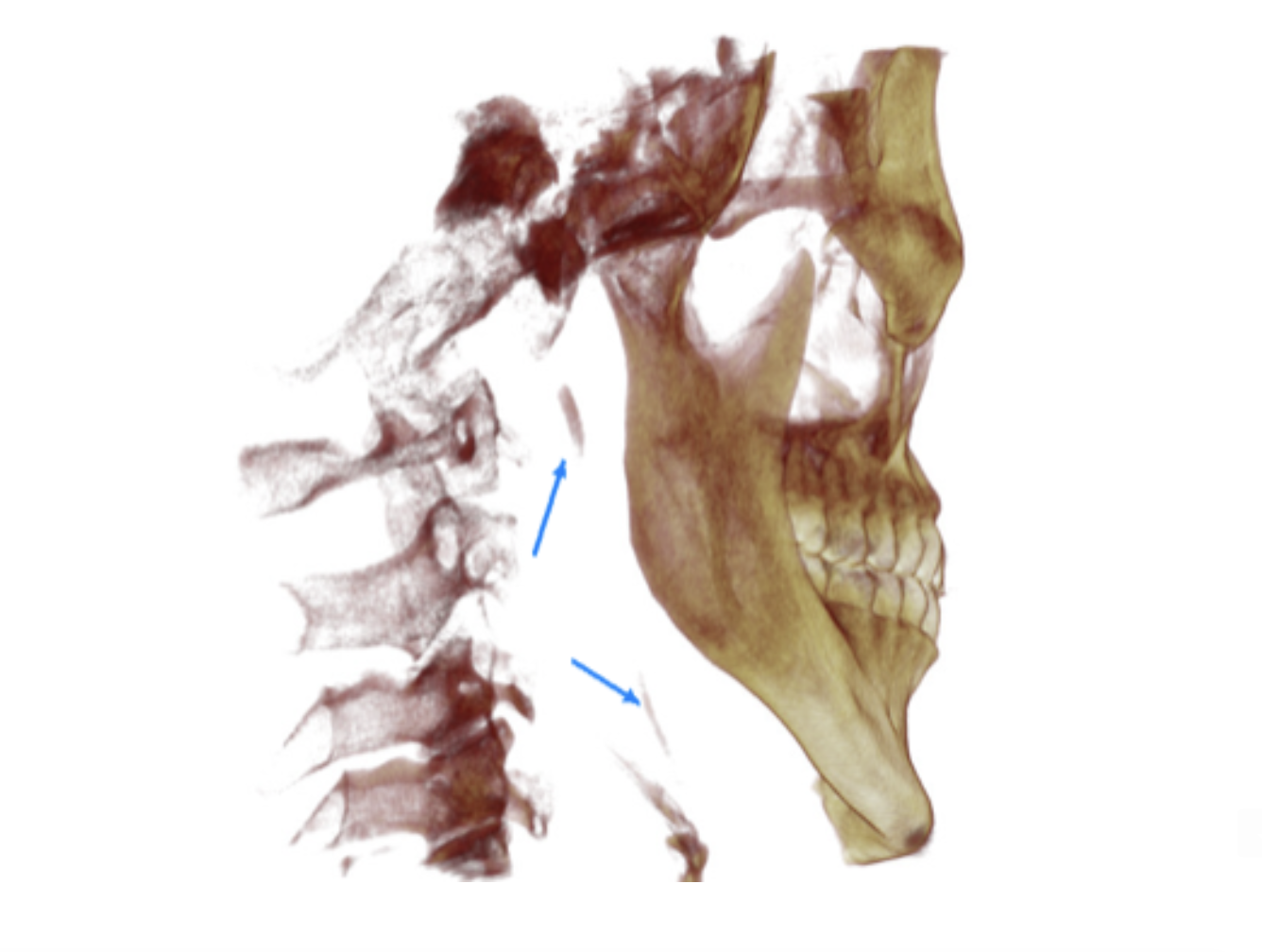
Calcified Stylohyoid Ligaments Due To Tension from the Pharyngeal Dilator Muscles Attached to the Hyoid Bone: Indicates Chronic Efforts to Keep the Airway Open.

Severely Deviated Nasal Septum
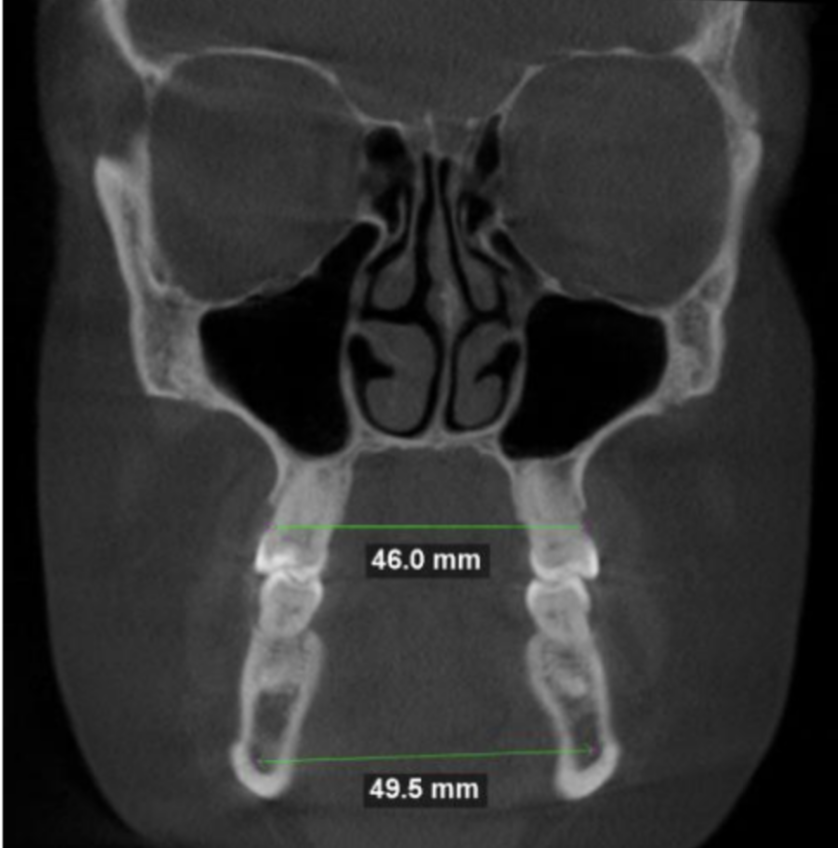
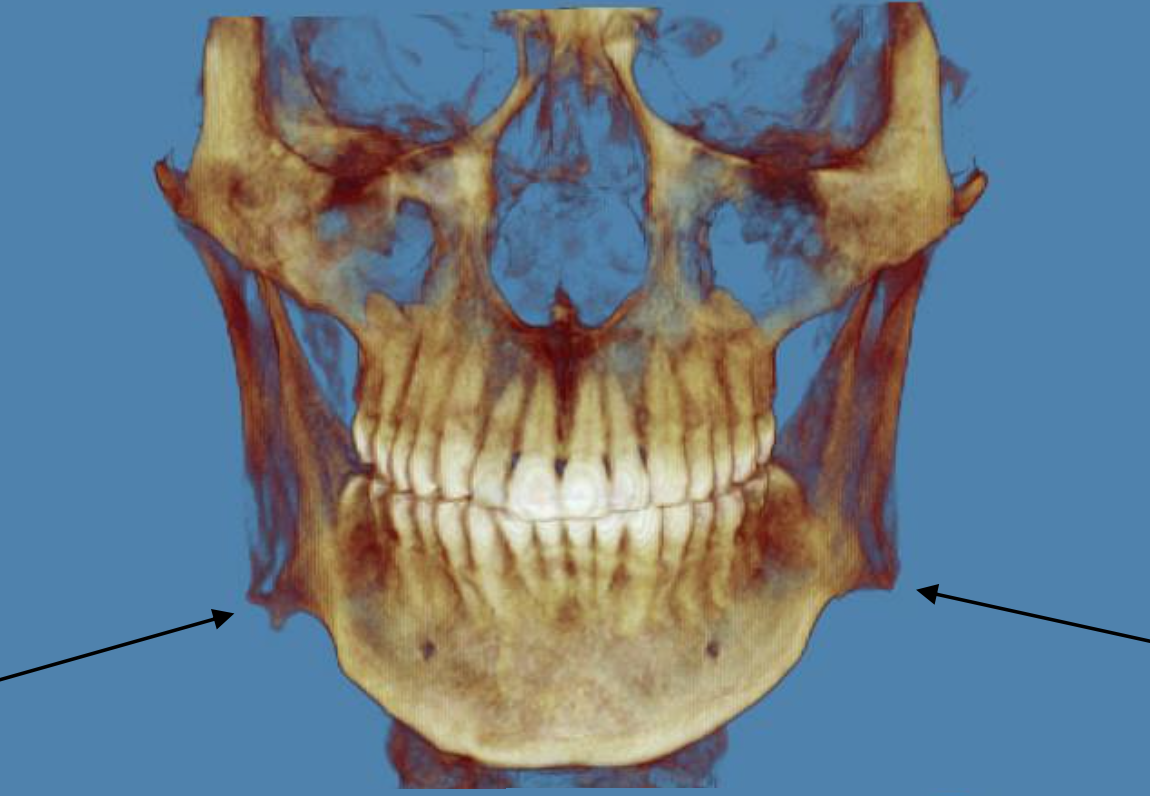
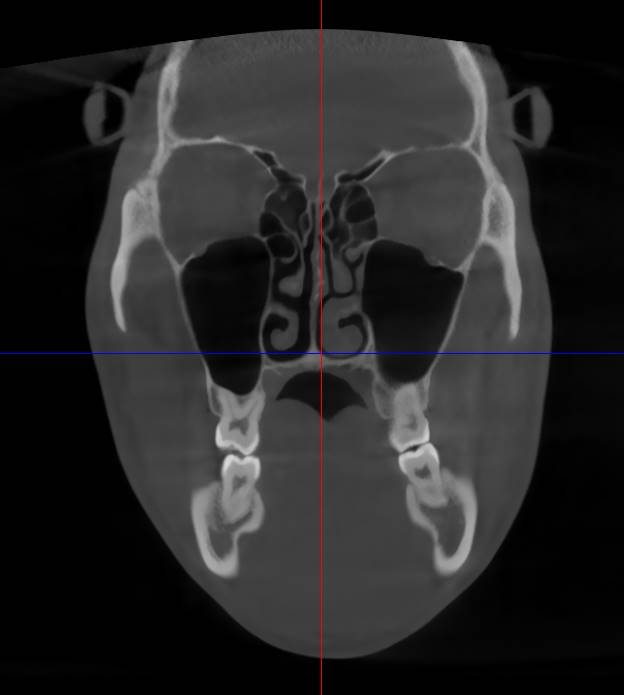
Severe Tranverse Maxillary Deficiency: The Maxilla Should be Approximately 9 mm Wider Than the Mandible at the First Molar Level.

Tonsil Stones Due to Chronic Mouth Breathing

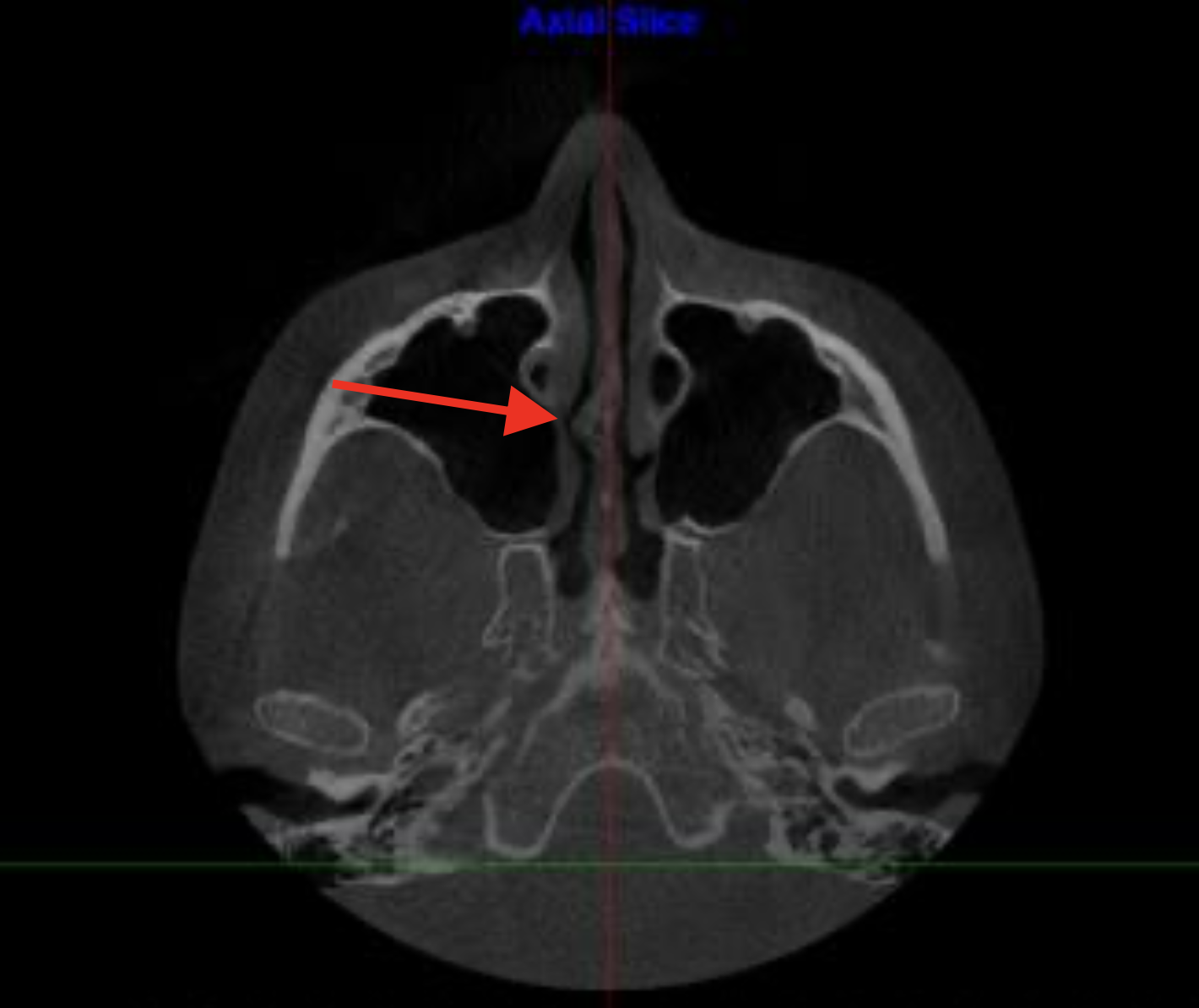
Bi-Lateral Nasal Valve Collapse Exacerbated by a Left Nose Ring
Substantial Transverse Maxillary Deficiency of Approximately 7 mm.

Calcified Genial Tubercle: Tongue Muscle Overactivation to Open a Compromised Airway Causes Calcification of the Tendon Insertion at the Genial Tubercle.

Right Nasal Valve Collapse
Flaring Gonial Angle Flaring and Notching from decades of overactive jaw muscles trying to maintain an open airway.

Mucous Retention Cyst in Right Maxillary Sinus
Shrek

Narrow Pharyngeal Airway at Tongue Base

Loss of Cervical Spine Lordosis Due to a Forward Head Posture Compensating a Restricted Airway

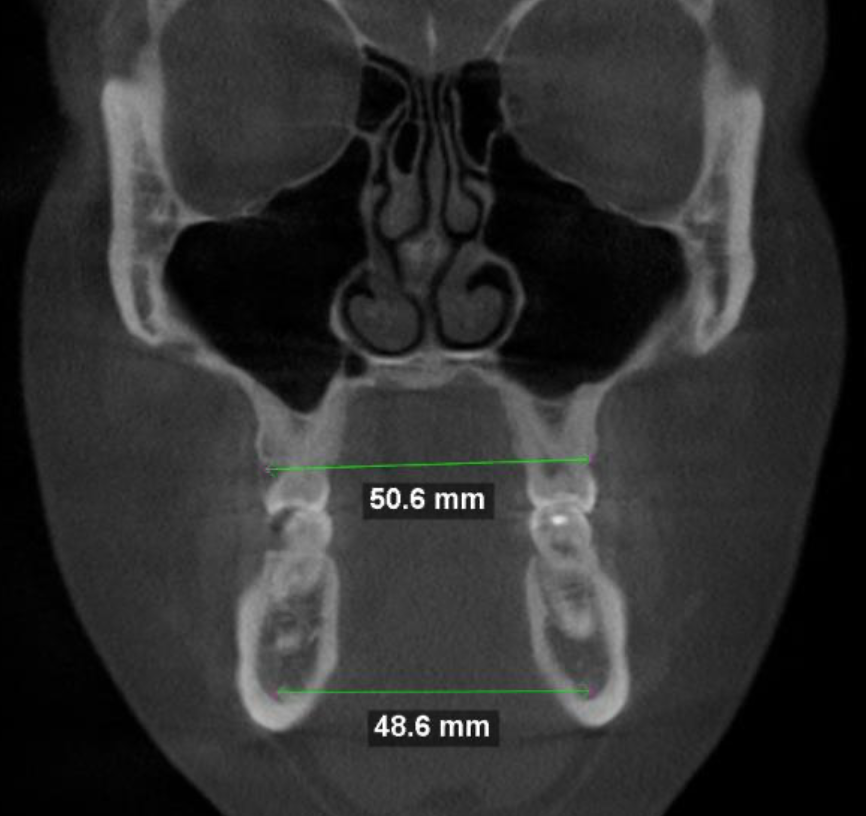
Oral Appliances May Not Improve Airway Volume and Could Cause Side-to-Side Narrowing With Mandible Advancement In a Narrow, Ovoid-Shaped Pharyngeal Airway.
Bone Spur Causing Nasal Obstruction

Bone Spur Causing Nasal Obstruction

Oral Appliances May Expand Airway Volume with Mandible Advancement in a Wide, Flat Pharyngeal Airway.
Excellent Transverse NasoMaxillary and Mandibular Width

Tonsil Stones Due to Chronic Mouth Breathing
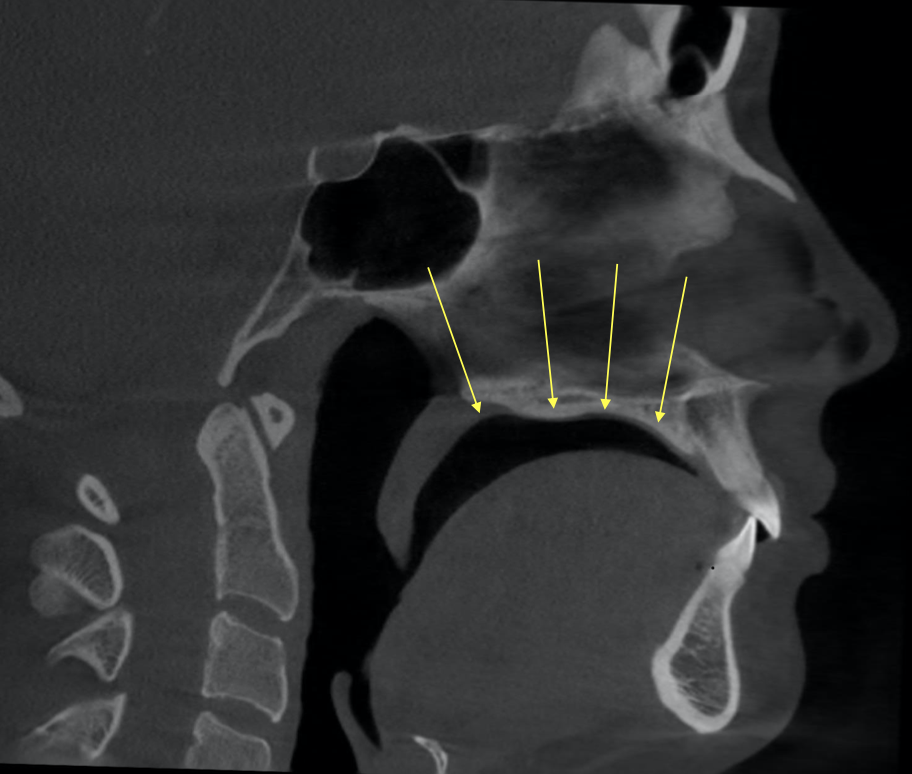
Low Tongue Posture. Black Space Represents Air Between the Tongue and Upper Palate.

Palatine Tonsil Hypertrophy
Laboratory sleep testing with carbon dioxide monitoring, performed in your home, may be necessary to evaluate additional sleep-disordered breathing such as hypoventilation.
We typically begin with sensitive home sleep testing with peripheral arterial tonometry to quantify your sleep patterns and evaluate sleep-disordered breathing and sympathetic arousal frequency.
Sleep apnea is a traumatic brain injury. We offer sophisticated testing to elucidate areas of brain imbalance. A brain map can pinpoint which brain areas are hyperactive and hypoactive and assess which networks between brain areas are improperly functioning. Our goal is to restore brain function.
Fortunately, a plethora of therapeutic treatment options are available for sleep-disordered breathing. Unfortunately, many individuals are unsuccessful with standard therapy. We direct individualized treatment toward sleep-disordered breathing, depending upon your age, anatomy, and life experience, and as exampled below:
Obstructive Sleep Apnea
Lifestyle modifications (e.g., alcohol, tobacco, sedatives)
Weight loss
Positional therapy
Zzoma OSA
Positive airway pressure
Mandibular advancement splint
Allergy evaluation and treatment
ExciteOSA neuromuscular stimulation device
iNAP
Nasal surgery
Palate expansion
EASE, FME, MSE, Double MSE, MARPE, Custom MARPE, MIND
Rhinomanometry provides a quantitative measure of nasal airway resistance that can be used to investigate positive airway pressure intolerance and the indication for nasal surgery.
Capnography to evaluate for hypocapnia causing apnea exacerbation
Capnotherapy to restore eucapnia
Maxillomandibular advancement
Inspire hypoglossal nerve stimulator
We use Sleeptracker-AI to assess the effectiveness of sleep apnea treatment and identify areas where it may fall short. Sleeptracker-AI is clinically validated to accurately monitor sleep patterns, cardiovascular and breathing metrics, breathing anomaly index, and other biometrics. The accuracy of the Sleeptracker-AI system has been validated in collaboration with Stanford Sleep Medicine, ensuring that the data collected is reliable and comparable to gold-standard polysomnography measurements.
Sleep apnea is associated with reduced airway muscle tone, especially during sleep. Respiratory muscle weakness can exacerbate airway collapse and breathing disturbances. Maximum Inspiratory Pressure and Maximum Expiratory Pressure are respiratory muscle strength measures that are helpful for managing obstructive sleep apnea and insomnia. If testing reveals respiratory muscle weakness, treatments targeting inspiratory and expiratory muscle strength (i.e., respiratory muscle strength training) may help improve apnea. This holistic approach ensures accurate diagnosis and optimizes treatment.
Respiratory Muscle Strength Training (RMST) is a specialized form of exercise aimed at improving the strength and endurance of the muscles involved in breathing, including the diaphragm, intercostal muscles (between the ribs), and accessory muscles. RMST typically involves targeted exercises and the use of resistance devices that create resistance to breathing, which can enhance both inspiratory (breathing in) and expiratory (breathing out) muscle strength.










